What do these guys have in common?
Telly Savalas
Frank Zappa
Francois Mitterrand
Johnny Ramone
Timothy Leary
Merv Griffin
… and about 30,000 lesser-known people over the past year.
They’re all men and they all died of prostate cancer.
Life and Lemons
I have a personal policy of not over-sharing on social media. I wouldn’t have shared this either except that I felt an obligation to post a public service announcement. A PSA about PSA.

In 2021, a couple of friends were suddenly stricken by serious diseases. I decided that 30 years was long enough not to have had a complete physical. So I contracted with a concierge medical provider, One Medical on Smith Street in Brooklyn. I booked a wellness visit for the following week. I got a soup-to-annisette exam: history, full blood panel, BP, PulseOx, EKG, the works. A few days later I received the not unexpected news via One Medical’s app.
If I had ignored annual maintenance on my car for thirty years I would presume there would be some issues. And there were with me too. The one highlighted out-of-range number of concern was my PSA. It was 10 ng/mL. It should be less than 4 for a person of my age. A couple of hours later I got a call from my One Medical PCP, Dr. Elizabeth. She was concerned and was referring me to Mount Sinai Urology in Brooklyn Heights for followup in ten weeks.
PSA means Prostate-Specific Antigen. It’s a protein produced by both healthy and diseased prostates. It has become a standard test in blood panels in men over 50. It’s the relative level that’s the determinate. A PSA under 4.0 is generally considered normal. There are exceptions but a PSA greater than 4 is a warning that something is amiss. It might be cancer, prostatitis, benign prostatic hyperplasia or some other medical term I had no clue about. Dr. Elizabeth’s words pushed all my medium range plans off the table. She said that a PSA of 10 was a strong indicator for prostate cancer.
Ten weeks later, I went to my 9am appointment at Mount Sinai. After hanging out in the lobby for 45 minutes all of us 9am-and-earlier patients were told that none of the urologists had shown up yet that morning due to some weather event in the burbs. We were told that someone would call to reschedule our appointments.
It was the first sign of Mount Sinai’s questionable institutional bedside manner. In the weeks that followed no one from the Urology office contacted me about a new appointment so it just slipped from my attention until six months later when I learned that a friend of mine had just been diagnosed with prostate cancer. That woke me up. I contacted the Urology practice but was told that I would have to go through the referral process all over again. Strike Two for Mount Sinai.
I decided to wait until my Summer 2022 physical to get a new referral. The blood panel from that encounter revealed that my PSA had risen to 15. My PCP was angry at Brooklyn Mount Sinai’s response so she made a new referral to Mount Sinai/Union Square in Manhattan. The young urologist at that visit told me that there was >50% probability of cancer. I was scheduled for an MRI and a biopsy. A month later both confirmed a one square centimeter mass and a Gleason score of 3+4.
Prostate Cancer Is A Sneaky Bastard
I read that Frank Zappa had complained to his doctors about urination problems for a decade before he was diagnosed with inoperable prostate cancer in 1990. That was surprising to me because I had no symptoms other than that PSA and you don’t actually feel an elevated PSA. PSA testing didn’t become a standard line item on male blood panels until around 1989. Before then it was a difficult cancer to detect. Zappa was ahead of his time in more ways than his music.
Despite prostate cancer being one the most curable cancers many men die of it because by the time physical symptoms do appear it’s often too late to do anything about it. By then it’s often metastasized. Dr. Elizabeth was very insistent about me taking this more seriously. She said that she had a prostate cancer patient where the cancer had metastasized into his shoulder. That’s when he first noticed that something was wrong. For him, the war was over.
Mount Sinai/Union Square referred me uptown to the main hospital on 101st and Madison Ave. My urologist was proud to tell me that he had snagged an appointment for me with a top guy at Mount Sinai Urology, a man he described as almost the Robert Jarvik of prostate medicine. He was one of the top three prostate surgeons in the country, he said. I felt that I was in good hands. I’m not mentioning full names here for a reason.
I saw Dr T in November 2022. Nevertheless, I’m a big “get multiple estimates” guy so I also made consult appointments with the chief of radio-surgery at Sloan-Kettering and with Maimonides in Brooklyn because of its years of touting Cyberknife as a prostate cancer treatment on 1010WINS.
I’ll add another strike to Mount Sinai’s bedside manner. As many as half my visits over the next few months, which occupied at least three hours out of my work day, could have been two-minute telehealth calls. There was no medical reason for me to be present or to spend 150 bucks on Ubers. It showed a lack of concern for patients and especially for a pandemic that was heading into another potentially deadly winter.
Anyway, while building my research I found that there are several ways to treat prostate cancer:
- Conventional surgery, like what Mount Sinai offered me. These days it’s typically laparoscopic robotic surgery via a Da Vinci system.
- Linear accelerator surgery, a/k/a Cyberknife and its branded variants. It’s a non-invasive, robotic treatment called stereotactic radiosurgery (SRS) using a highly focused radiation beam hitting the tumor from thousands of unique angles with minimal damage to surrounding tissue. Treatment is usually accomplished in five 30-40 minute sessions. It’s also called SBRT (Stereotactic Body Radiation Therapy)
- A more conventional lower dose radiation treatment which can take as many as 45 sessions. It reportedly has the fewest post-treatment complications with the additional risk of radiation-induced cancer.
- Finally, do nothing. If your PSA is elevated but stable, you’re over 65 and the tumor is found to be a slow-growing type, you’ll probably die of something else long before prostate cancer punches your ticket.
The Odds: One In Seven
Why would anyone do nothing about it? It’s cancer! The reason is because the treatments each carry their own set of risks, primarily incontinence and impotence which may be permanent. The prostate lives in a crowded neighborhood and in a tightly woven basket of important nerves. Several other organs can be potentially damaged by friendly fire as well. It’s the reason why “do nothing” is a common option in Group 1 prostate cancer. The cure can be worse than the disease.
As is usually the case when someone is diagnosed with serious disease, I cast a net among my acquaintances looking for others who had had prostate cancer. I needed help making a decision on a formal course of treatment. Prostate cancer is something that guys don’t usually bring up with each other in casual conversation. I was surprised by the number of men I’d known for years who had had prostate cancer, a couple of them having been diagnosed as young as their late 30s. I learned that one in seven men will get prostate cancer. Those numbers comport with what I found in my own anecdotal demographic. One in 33 will die from it.
In other words, if you are as irresponsible with your medical health as was I, you’re reading this article and there are six more “like mes” doing likewise, one of you had, already has or will have prostate cancer.
I spoke with several men who had gone the scalpel surgery route, Most said they wished they hadn’t. Granted, radical prostatectomy has made giant leaps in the past 20 years since the oldest procedure among my group of acquaintances. But one was wearing adult diapers two years later and another was still impotent. Those who did the radio-surgery route were upbeat about it. What also turned me off to a surgical treatment was that one of those men had Dr. T as his surgeon. Oh boy. More about that coming up.
That’s not to say there aren’t post-treatment risks with radio-surgery. They just tend to be less permanent. Radio surgery is conducted as an out-patient procedure. Surgical prostatectomy patients typically go home with a catheter and a pee bag for at least a week. Oh boy again.
That’s why I found myself at Sloan-Kettering investigating their Cyberknife variant called SHARP. But the doctor at my consult was a rather dour and unfriendly sort and said I wasn’t a candidate for it because I had an anterior tumor that their system couldn’t treat.
Rats.
I Made My Decision. And Dodged a Bullet.

I was stunned. I could see a similar reaction in the faces of his team who obviously weren’t expecting to hear that either. This guy had seen me since November, had his minions run multiple physical exams, MRIs, CTs, and made me jump through 11th Hour hoops with my own PCP just to make that surgery date. My height, weight and BMI were on the front page of my medical chart for months. And not once had he ever said that he wouldn’t operate at my then-extant COVID weight.
Needless to say, I was pissed. Also needless to say, I fired him. But now I was back to Square One and my last PSA was 16. It was getting worse.
With the help of my One Medical PCP and a lot of Googling, I found Dr. Christopher Barbieri at NY Columbia Presbyterian/Weill-Cornell on E.68th Street. I looked up his Healthgrades reviews which were uniformly positive. Five stars out of five. It’s also where I saw Dr T’s reviews which weren’t as flattering, including an accusation that he farmed out surgery to less experienced associates. So he wasn’t the best after all. I’m sure he’s a good surgeon but I wouldn’t want to run his practice’s complaint department.
I got the consult appointment with Dr. Barbieri in a few days and instantly liked him. He was a scalpel surgeon. I told him that while I preferred radio-surgery treatment I was advised that I wasn’t a candidate for it. He glanced at my MRIs and said, “No, you’re a candidate. Let me set up a consult with our Radiation Oncology Dept and Dr. Himanshu Nagar“. I had a telehealth call with Dr.Nagar two days later. Two days after that I had back-to-back CTs and MRIs to program their SBRT and received three tiny tattoos used for target alignment. I also have to say that NY Presbyterian’s infrastructure and patient care methodology seemed to be a generation newer than Mt Sinai’s. For instance, they insisted that all non-essential patient encounters be telehealth.
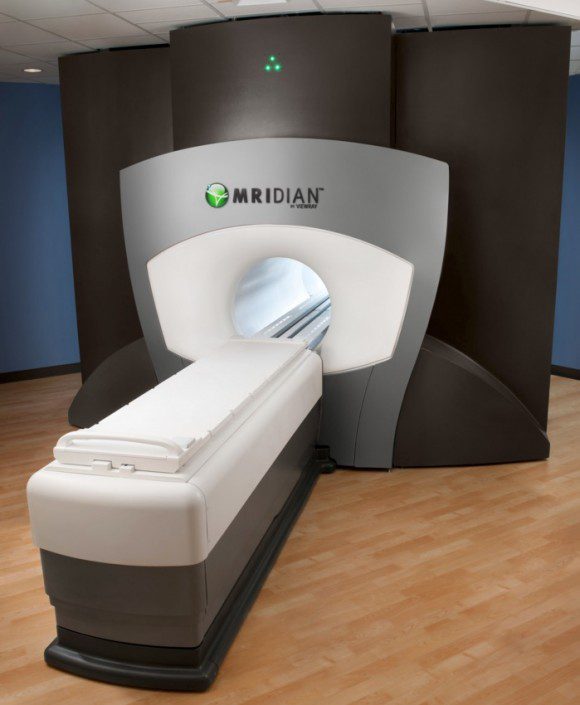
The huge machine which costs as much as a luxury corporate jet lives in its own thousand square foot room and allows the operator to see MRIs in real time with the treatment. It also offers patients their choice of Spotify music playlists to listen to and travelogues to watch during treatment. That was huge with me because I’m claustrophobic. I normally need 5mg of Valium to climb into one of these tubes.
I had the first treatment on June 12, 2023. After Treatment #5 the MRI confirmed that my cancer was a cinder. So was my prostate and one suspicious lymph node.
There were some minor post-surgical complications but none were bothersome. The most pronounced one was physical tiredness. I was told that they could get worse over the next two weeks before they reverse themselves. It didn’t get worse and it was nothing compared to the blotchy stress hives I’ve had to deal with since this process began.
Grad School
Three weeks later I returned to NY Presbyterian, this time in Park Slope, Brooklyn, for tests and four months of post-surgical infusion treatment under the care of Dr. Peter Gregos, another young, well-informed and friendly guy. Before the first infusion (just a single shot) my PSA had dropped from 17 to 7 which was a good sign. The infusion is an anti-hormone to drop testosterone production to zero.
I learned that prostate cancer feeds on testosterone. Contrary to Howard Stern’s regular rants about masturbating 30 times a month to prevent prostate cancer, testosterone actually fuels the growth of prostate cancer cells. In my case I was prescribed three monthly shots of Firmagon followed by one shot of Eligard at Month #4.
I was warned by my prostate-suffering friends that this treatment could also have some nasty side effects, loosely like male menopause plus tiredness and weight gain.One of them said that he had to lock himself in his office for 48 hours after his shots because he wanted to still be married at the end. His infusion was for 18 months, Mine was considerably shorter. Again, technology.
I stopped drinking alcohol for the tiredness and enrolled in Nutrisystems for the weight gain. I definitely felt these side effects, most notably the crushing tiredness. Nutrisystems just fought a holding action against the treatment. I’ve always been a night owl but I found myself crashing at 9pm and awake again at 3am. It’s fortunate that I have a flexible remote job with a health-sector company run by MDs and MPHs. I got a lot of tacit support for my weird work hours.
I’m on my second to last hormone shot now and my PSA after the last one dropped to 3.8mg/mL.
Success! And all the equipment still works fine!
Concluding…
Look, I know that going to doctors is a PITA. It’s why it took me 30 years between wellness visits. I have a touch of ADD and can’t stand being made to wait three months for an appointment only to spend two hours in a waiting room only to be referred out to yet another practice and then another. One Medical fixed that for me and it may well have saved my life. Quick appointments, very low wait time, on-site lab, and 24/7 consulting via their branded app.
Amazon acquired One Medical a few months ago. I hope they don’t ruin it. The One Medical app also (optionally) ties seamlessly with Amazon Pharmacy so your medications are automatically refilled and delivered to your house.

Back to the closing point: prostate cancer is no joke. In the hierarchical world of cancers, it’s not pancreatic adenocarcinoma or glioblastoma. It’s a low, slow ball over the plate for experienced doctors to deal with provided that it’s caught in time. Since it’s part of the blood panel in the annual wellness visit it couldn’t be easier to detect. You just have to do that annual wellness visit.
End of PSA.
